Genetic testing for salivary gland cancer (SGC)
Salivary gland cancers are malignant neoplasms of the salivary glands that differ in their morphologic structure.
Salivary gland malignancies are rare and account for approximately 6-8% of all head and neck cancers. Salivary gland cancers have a higher incidence in relatively young people (15-40 years of age) and women. However, some forms of salivary gland malignancies such as ductal carcinoma (DC) and metastatic squamous cell carcinoma have an increased prevalence in older men.
Among the different histologic types, the most common are (see table):
- mucoepidermoid carcinoma (MEC)
- adenoid cystic carcinoma (ADCC)
- acinic cell carcinoma (ACC)
Salivary gland cancer (SGC) is a multifactorial disease and involves complex environmental and genetic interactions.
The factors below can serve as triggers for the development of RSG:
- ionizing radiation
- chemical exposure
- obesity
- autoimmune diseases
- viral infections (such as Epstein-Barr virus in lymphoepithelial carcinoma)
Abnormalities in tumor suppressor genes and oncogenes, chromosomal translocations can also contribute to the development of salivary gland neoplasms (both benign and malignant).
Salivary Gland Anatomy
The composition of the salivary gland acinus depends on the anatomical location. Thus the parotid gland consists predominantly of serous acinar cells, the submandibular gland consists of a mixture of serous and mucinous cells, and the hyoid gland/small salivary glands are composed entirely of mucinous cells. Malignant neoplasms can arise from any of the above cell types (see table).
A general rule of thumb is that the smaller the gland, the more mucinous cells and the higher the likelihood of malignancy forming in that gland.
Symptoms
The most common symptom of SGC is a painless mass in the parotid gland or neck.
Late-stage malignant neoplasms of the hyoid gland may manifest as a mass on the floor of the mouth. Pain, a rapidly growing mass, facial weakness, or lingual weakness/paresthesia (in the case of a hyoid tumor) are signs that usually indicate an urgent need to seek medical attention.
Diagnosis
Fine-needle aspiration biopsy (FAB) is commonly used to evaluate salivary gland lesions.
FAB is favored for several reasons:
- It is a rapid and minimally invasive technique with high diagnostic sensitivity and specificity.
- FAB allows sufficient material to be taken for subsequent ancillary studies such as IHC, FISH, and flow cytometry.
- In patients with inoperable disease or who are recommended to proceed to primary systemic therapy, cytologic material can be used for molecular genetic studies to identify potential targets of targeted therapy.
Clinicopathologic features of commonly encountered primary salivary gland neoplasms
- Мукоэпидермоидная карцинома (МЭК)
- Ацинарноклеточная карцинома
- Карцинома-плеоморфная аденома (эПА)
- Аденокистозная карцинома
- Секреторная карцинома
- Карцинома слюнных протоков
- Полиморфная аденокарцинома
- Внутрипротоковая карцинома (карцинома вставочных протоков)
- Эпителиально-миоэпителиальная карцинома
- Базальноклеточная аденокарцинома
- Гиалинизирующая светлоклеточная карцинома
- Микросекреторная аденокарцинома
- Муцинозная аденокарцинома
- Склерозирующая микрокистозная аденокарцинома
Treatment of salivary gland cancer
Surgical treatment
АAdequate surgical resection is the most effective treatment for salivary gland cancer. However, the extent of surgical intervention is one of the most widely debated topics in surgical oncology of head and neck tumors, especially regarding the extent of gland resection.
Radiation therapy
Radiation therapy (RT) is crucial in the treatment of of salivary gland malignancies. Usually it is administered adjuvant LT after tumor resection for standard postoperative indications, including the presence of tumor cells in the resection margins, spread to the lymph nodes, peripheral lymph nodes, and peripheral lymph nodes. lymph nodes, perineural invasion, and specific histologic subtypes. LT is also used in patients with inoperable tumors or in patients with contraindications to surgery. treatment. Some types of salivary gland malignancies salivary gland malignancies tend to spread to the cranial nerves, which leads to additional difficulties for determining the target volume of radiation therapy, as often planned radiation therapy to the cranial nerves cranial nerves. In situations where the target LT volume is approaching critical normality, new radiation therapies can be utilized. newer radiation therapy modalities such as proton therapy.
Chemotherapy
Unlike head and neck squamous cell carcinoma, there are few prospective data for SGC to inform clinicians about the use of chemotherapy in addition to radiation therapy (RT) after surgical resection. Salivary gland carcinomas are a heterogeneous histologic group, and large clinical trials are difficult to perform in this setting. Retrospective studies have shown mixed results with adding postoperative chemotherapy to RT. Because of this, the use of chemotherapy is often ambiguous. In practice, a decision is often made based on the clinical judgment of the treating specialist and discussion with the patient. Pathologic features such as positive resection margins, histologically highly differentiated tumors, and multiple affected lymph nodes are often regarded as poor prognostic markers and increase the likelihood of prescribing systemic treatment.
Immunotherapy
The global cancer communities recommend the involvement of patients with metastatic salivary gland cancer (mSCG) in clinical trials, given the limited options of standard systemic therapy for patients with SGC.
The PD-1 receptor inhibits T cell function by binding to its ligands PD-L1 and PD-L2. In retrospective studies, PD-L1 expression in 22.8% of mSCG is associated with worse progression-free time and overall survival.
Several large clinical trials involving patients with SGC have shown the potential efficacy of prescribing checkpoint inhibitor therapy in patients with metastatic or inoperable RA and PD-L1 expression.
Targeted therapy
Anti-HER2 therapy
It is known that clinically more aggressive SGC often overexpresses or demonstrates amplification of the HER-2/neu proto-oncogene. Because SGC is histologically similar to breast invasive ductal carcinoma, HER2 expression is potentially important for salivary gland tumors (both primary and metastatic) as well. Larger studies evaluating several histologic types of salivary gland cancer for HER2 overexpression have shown a low overall frequency of overexpression, ~17%. Still, for some histologic subtypes, such as ductal carcinoma, mucoepidermoid carcinoma, and carcinoma ex pleomorphic adenoma, HER2 overexpression positivity ranged from 21% to 83%.
Results of clinical trials of HER2 therapy in patients with metastatic or inoperable SGC showed a good response to therapy (47-70%) and increased time without disease progression (9-14 months).
Androgen deprivation therapy
AR is a nuclear receptor for steroid hormones expressed in several human tissues, and its major ligands are testosterone and 5α-dihydrotestosterone. AR regulates the transcription of several effector genes through direct interactions with DNA. As with HER2, AR expression measured by IHC varies among the different types of SGC and is most frequently detected in ductal carcinomas (64%-98%). the frequency of AR expression in other salivary gland cancer subtypes varies from 0-30%.
Androgen deprivation therapy (ADT) is often used to treat patients with SGC and AR expression in the tumor. In retrospective studies of patients with AR-positive salivary gland cancer treated with the oral antiandrogen bicalutamide with a gonadotropin-releasing hormone agonist, 42-65% of patients with SGC demonstrated response to therapy, and the median progression-free time increased to 9 months.
Targeted therapy based on molecular targeting studies
As mentioned above, one of the major challenges in treating salivary gland malignancies is that they are rare entities encompassing a wide variety of diseases, including more than 20 histologic subtypes. This complexity predictably extends to the biology underlying these diseases.
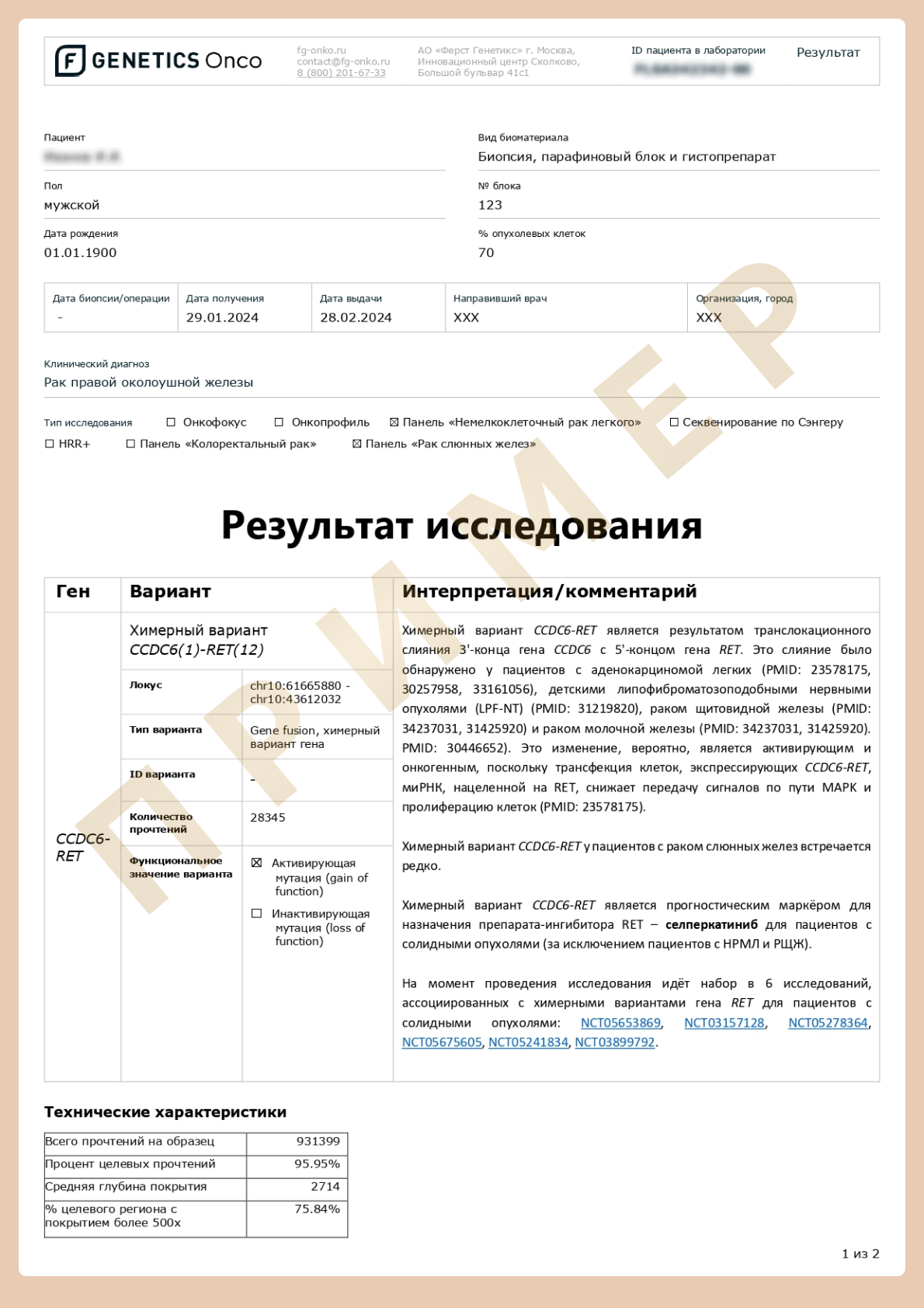
The growing importance of molecular profiles for diagnosis, prognosis, and therapy selection in SGC is partly reflected by including molecular markers in the World Health Organization definitions for certain histologic subtypes of SGC. Among the most important for therapy selection are NTRK3 and RET rearrangements for secretory and intraductal carcinomas, respectively, and AKT1 mutations for mucinous adenocarcinomas. There are currently approved drugs for the treatment of RET (selpercatinib, pralcetinib) and NTRK (entrectinib, larotrectinib) rearrangements, as evidenced by high response rates and clinical efficacy for patients with tumors containing the corresponding genetic alterations.
What is genetic testing for salivary gland cancer?
NGS-based analysis involves the study of genes that coincide with the clinical use of approved targeting drugs and drugs from prospective clinical trials for salivary gland cancer.
Changes in these genes lead to tumor development and are used as diagnostic, prognostic, and predictive cancer markers.
The study involves the analysis of 15 genes
Indications for testing
patients diagnosed with salivary gland cancer for:
- Therapy selection
- Monitoring and therapy correction in case of recurring disease
- Involvement in clinical trial programs
How to request the Salivary gland cancer test?
Download and fill out the informed consent form
A courier will collect histological material and take it to the laboratory free of charge.
First Genetics Laboratory
Specialists
Years of experience in genetics, laboratory diagnostics and bioinformatics
Confidentiality
All data is strictly confidential and cannot be passed on to third parties
Time frame
Results ready in a short time
Security
Extensive control at each stage of testing
No delivery fees
Free delivery of biomaterial across Russia
Charities
Email info@f-genetics.com for information